Introduction
Malaria remains one of the most significant public health challenges in sub-Saharan Africa, with Kenya bearing a substantial burden of the disease. As a tropical country with diverse ecological zones conducive to the proliferation of the Anopheles mosquito—the primary vector for malaria transmission—Kenya reports millions of cases annually, disproportionately affecting vulnerable populations such as children under five and pregnant women. According to the World Health Organization (WHO), Kenya accounts for a significant portion of the global malaria burden, with an estimated 37.2 million people at high risk of infection (WHO, 2023). Despite concerted efforts over the decades, including the implementation of national strategies and international partnerships, malaria continues to pose severe health and economic challenges, thwarting progress toward sustainable development goals.
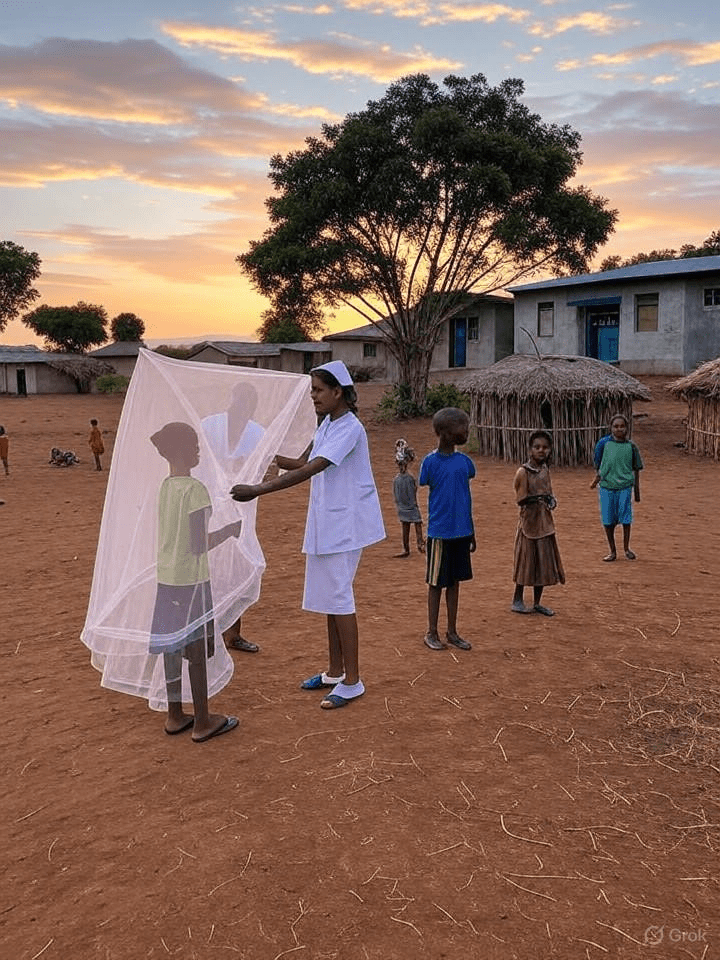
The fight against malaria in Kenya is rooted in a complex interplay of biological, environmental, social, and economic factors. While progress has been made through interventions such as insecticide-treated nets (ITNs), indoor residual spraying (IRS), and artemisinin-based combination therapies (ACTs), the path to eradication remains fraught with obstacles. These include insecticide resistance, increasing outdoor transmission, inadequate surveillance systems, and disruptions caused by global health crises such as the COVID-19 pandemic. Additionally, regional disparities in healthcare access and the impact of climate change further complicate control efforts.
This article examines the challenges and strategies for battling malaria in Kenya, with a focus on the current state of interventions and the barriers to achieving eradication. Through a situational analysis, literature review, and discussion of key issues, the paper aims to provide a comprehensive overview of the malaria landscape in Kenya. It also offers actionable recommendations to guide policymakers, researchers, and public health practitioners in their efforts to eliminate malaria. By addressing both the structural and contextual factors influencing malaria control, this paper seeks to contribute to the global discourse on malaria eradication in high-burden countries.
Situational Analysis
Malaria in Kenya exhibits significant geographical and demographic variations, with transmission intensity varying across different epidemiological zones. The coastal and lake regions, including areas around Lake Victoria, are hyperendemic zones with year-round transmission, while highland areas experience seasonal outbreaks exacerbated by climatic variability. The Kenya Malaria Strategy (2019–2023) reports that approximately 70% of the population remains at risk, with children under five and pregnant women facing the highest morbidity and mortality rates (Kenya Ministry of Health, 2019). In 2016, the baseline year for the current strategy, there were over 8 million reported cases, and the goal was to reduce both incidence and deaths by 75% by 2023 through an investment of Kenyan Shillings 61.9 billion (Njau et al., 2023).
Despite progress in some areas, such as increased distribution of ITNs and access to diagnostic testing, several challenges persist. Insecticide resistance among Anopheles mosquitoes has emerged as a critical barrier, reducing the efficacy of vector control measures like ITNs and IRS. Studies indicate that resistance to pyrethroids, the most commonly used insecticide class, is widespread in western and coastal Kenya (Ochomo et al., 2020). Additionally, there has been a notable shift toward outdoor biting behavior among mosquitoes, which diminishes the impact of indoor-focused interventions.
Socioeconomic inequalities further exacerbate the malaria burden. Rural communities, where access to healthcare facilities is limited, often experience delayed diagnosis and treatment. This is compounded by urban-rural disparities in the distribution of resources such as ITNs and trained health personnel. Environmental factors, including deforestation and water resource development projects, have also altered malaria transmission patterns by creating new breeding sites for mosquitoes. For instance, the construction of dams and irrigation systems in certain regions has been linked to increased malaria incidence (Keiser et al., 2005).
The COVID-19 pandemic introduced additional disruptions to malaria control programs in Kenya. Lockdowns and resource reallocation led to interruptions in the distribution of ITNs and access to treatment, resulting in reported increases in malaria morbidity in low- and middle-income countries (Weiss et al., 2023). This situation underscores the fragility of health systems in sustaining malaria interventions during overlapping health crises.
From an economic perspective, malaria imposes a substantial burden on Kenya’s economy. The disease contributes to lost productivity, high healthcare costs, and reduced household income, particularly in agrarian communities reliant on manual labor. A study published in the Malaria Journal highlights that malaria control and elimination efforts could yield significant economy-wide benefits, but regional disparities in implementation must be addressed to ensure equitable gains (Njau et al., 2023).
Literature Review
The body of literature on malaria in Kenya highlights both the successes of control programs and the persistent barriers to eradication. Early interventions in the 20th century focused on vector control through DDT-based IRS, which yielded significant reductions in malaria prevalence before resistance and environmental concerns halted widespread use (O’Meara et al., 2010). The introduction of ITNs in the late 1990s marked a turning point, with studies demonstrating a 50% reduction in malaria morbidity among children in high-transmission areas (Lengeler, 2004). Subsequent rollouts of ACTs as the first-line treatment further reduced mortality rates, particularly following the adoption of WHO guidelines in the mid-2000s (WHO, 2006).
Recent studies emphasize the evolving nature of malaria transmission in Kenya. The shift to outdoor biting by Anopheles mosquitoes, driven by selective pressure from indoor interventions, poses a significant challenge. Research by Bayoh et al. (2014) in western Kenya documented increased outdoor feeding behavior among Anopheles gambiae, necessitating the development of novel vector control tools. Additionally, insecticide resistance has been extensively documented, with resistance to multiple classes of insecticides reported across the country (Ochomo et al., 2020). This has prompted calls for integrated vector management (IVM) approaches that combine chemical, biological, and environmental strategies.
Climatic variability has emerged as a critical determinant of malaria transmission patterns. Studies indicate that temperature and precipitation directly influence mosquito breeding and parasite development, with warming trends in highland areas expanding the range of transmission (Pascual et al., 2006). A recent analysis published in the Malaria Journal modeled the effects of precipitation and temperature on malaria incidence in coastal and western Kenya, confirming a strong correlation between environmental factors and disease burden (Kamau et al., 2025).
Socioeconomic and systemic barriers are also well-documented in the literature. Rural communities face challenges related to poverty, limited health infrastructure, and cultural beliefs that hinder the uptake of interventions. For instance, a systematic review by Chuma et al. (2010) identified low awareness and misconceptions about malaria prevention as key barriers to ITN use. Furthermore, health system weaknesses, such as stockouts of antimalarial drugs and inadequate surveillance, undermine the effectiveness of control programs (Kibe et al., 2020).
The intersection of malaria with other global health challenges has gained attention in recent years. The COVID-19 pandemic disrupted routine malaria interventions, leading to reported increases in cases and deaths in sub-Saharan Africa. A systematic review by Weiss et al. (2023) highlighted the compounded burden of malaria in low- and middle-income countries during the pandemic, emphasizing the need for resilient health systems. Additionally, the emergence of antimalarial drug resistance, though less pronounced in Kenya compared to Southeast Asia, remains a looming threat that requires vigilant monitoring (Blasco et al., 2017).
Innovative strategies, such as the use of malaria vaccines, have begun to reshape the control landscape. The RTS,S/AS01 vaccine, piloted in Kenya since 2019, has shown promising results in reducing severe malaria among children, though coverage challenges persist (WHO, 2021). Complementary approaches, including community-based health education and digital health tools for surveillance, are also gaining traction as means to enhance intervention effectiveness (Kibe et al., 2025).
Discussion
The battle against malaria in Kenya is characterized by a complex interplay of biological, environmental, and structural challenges. Insecticide resistance and the shift to outdoor transmission by Anopheles mosquitoes underscore the limitations of traditional vector control measures such as ITNs and IRS. These biological adaptations necessitate the urgent development and deployment of alternative tools, such as next-generation insecticides, larval control methods, and genetically modified mosquitoes. While research into these innovations is underway, scaling up their implementation in resource-constrained settings remains a significant hurdle.
Environmental factors further complicate malaria control efforts. Climatic variability, driven by global warming, has expanded transmission zones into previously low-risk highland areas, while human activities such as deforestation and irrigation projects create new mosquito breeding sites. Addressing these environmental drivers requires cross-sectoral collaboration involving public health, agriculture, and environmental agencies to mitigate the impact of land-use changes on malaria transmission. Additionally, predictive modeling of climate-driven malaria trends, as demonstrated in recent studies, can inform targeted interventions in high-risk periods and regions (Kamau et al., 2025).
Socioeconomic disparities play a pivotal role in perpetuating the malaria burden in Kenya. Rural and marginalized communities, which often lack access to healthcare facilities and preventive tools, bear the brunt of the disease. This inequity is compounded by regional disparities in resource allocation, with urban centers receiving disproportionate attention compared to remote areas. Economic analyses suggest that malaria control and elimination could yield substantial benefits, including increased household welfare and productivity, but only if interventions are equitably distributed across epidemiological zones (Njau et al., 2023). Community engagement emerges as a critical strategy to address these disparities, ensuring that interventions are culturally appropriate and accessible to all segments of the population.
Health system challenges, including inadequate surveillance and workforce shortages, further impede malaria eradication efforts. Fragmented health information systems hinder real-time monitoring of malaria trends, delaying response to outbreaks. A recent study on strengthening health information systems in western Kenya highlighted the potential of digital innovations to improve data collection and analysis for malaria control (Kibe et al., 2025). However, the adoption of such technologies requires investment in infrastructure and